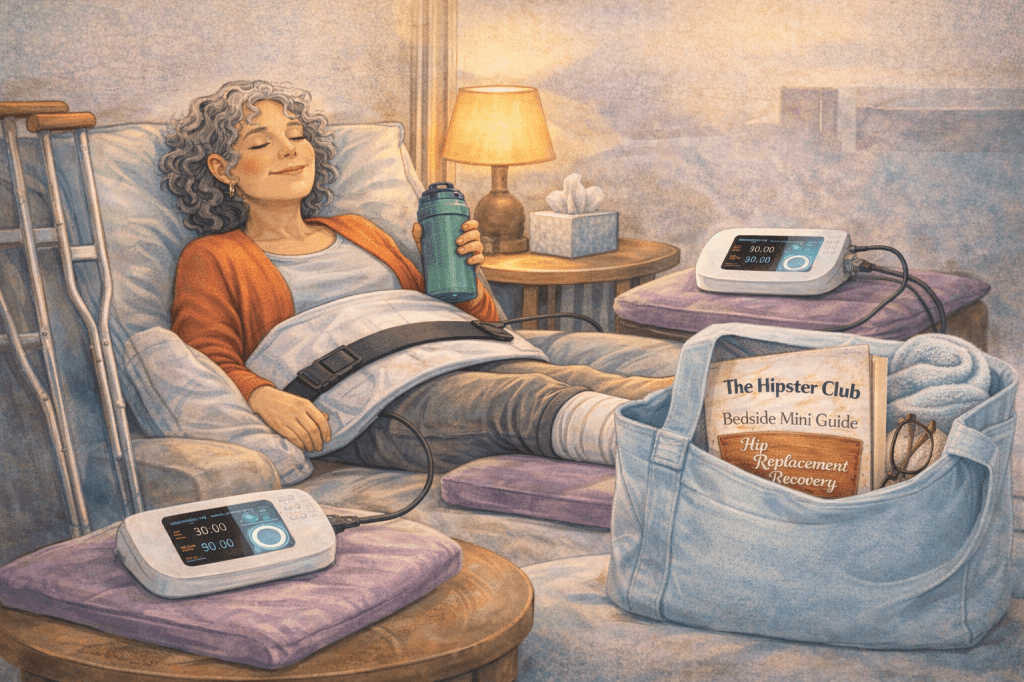
Reclaim Mobility, Confidence, and Your Life
Your Journey Begins
Hip and joint replacement is more than surgery—it’s a life-changing journey. Whether you’re preparing for your first hip or knee replacement, recovering post-op, or helping a loved one navigate this process, this guide gives you tools, insights, and support for every step.
What this guide covers:
- Nutrition & joint health
- Exercise & movement strategies
- Pain management & emotional support
- Prehab & preparation for surgery
- Community & peer sponsorship
- Complementary therapies, including PEMF
No one should face this journey alone. Let’s start together.
Nutrition & Joint Health
Healing begins inside your body. Proper nutrition reduces inflammation, strengthens bones, and supports tissue repair.
Anti-inflammatory foods:
- Fatty fish (salmon, sardines)
- Leafy greens (spinach, kale, broccoli)
- Berries and antioxidant-rich fruits
- Nuts and seeds
Supplements to discuss with your doctor:
- Vitamin D & calcium
- Magnesium
- Collagen or protein powders for tissue repair
Hydration: Essential for joint lubrication, toxin removal, and cellular repair.
Tip: Prep meals ahead of surgery for a stress-free recovery.
Exercise & Movement
Movement is medicine, but safety is key.
Early post-op (0–6 weeks):
- Gentle walking
- Short stretches
- Prescribed physical therapy exercises
Intermediate recovery (6 weeks–3 months):
- Low-impact cardio (swimming, cycling, elliptical)
- Light resistance exercises
Long-term recovery (3+ months):
- Yoga, Pilates, and walking clubs
- Maintaining strength, flexibility, and balance
- Returning to activities safely
Tip: Listen to your body—pain is a signal, not a reason to panic.
P Pain Management & Mental Health
Pain management:
- Follow your doctor’s advice for medication
- Use heat/cold therapy and TENS units
- Try PEMF therapy or acupuncture
- Mind-body techniques: meditation, visualization, breathing
Mental health support:
- Journaling progress
- Mindfulness and meditation
- Therapy or counseling
- Connecting with peer sponsors or community
Tip: Celebrate every milestone, no matter how small—mental recovery fuels physical healing.
Prehab & Preparing for Surgery
Preparation sets the stage for a smoother recovery:
Prehab exercises:
- Strengthen glutes, quads, and core muscles
- Gentle stretches for hip mobility
Home prep:
- Organize furniture for safe movement
- Install grab bars or non-slip mats
- Stock meals, water, and entertainment
Hospital survival kit:
- Comfy clothing
- Snacks
- Entertainment (books, tablet, music)
Tip: Being proactive reduces anxiety and sets you up for success.
Community & Sponsorship
Healing is better together. Support comes in many forms:
- Peer sponsors: Experienced patients guide and encourage you
- Online communities: Share questions, victories, and lessons learned
- Support groups: Local or virtual meetups for encouragement
Why it matters:
- Reduces isolation
- Offers real-world advice
- Provides hope and accountability
Tip: Join Hipster Club or a local support group—no one should recover alone.
Long-Term Care & Lifestyle
Your recovery doesn’t stop at discharge:
- Safe, low-impact activities maintain mobility
- Monitor for pain or new issues
- Social engagement supports mental health
- Treat your joint like a high-performance car—maintain and respect it
Tip: Long-term health is a lifestyle, not just a procedure.
Technology & Innovations
Modern advancements improve outcomes:
- Robotic-assisted or minimally invasive surgery
- Advanced prosthetic materials for durability and mobility
- Wearable tech and telehealth for recovery tracking
Tip: Ask your surgeon about the latest options—they can impact both recovery speed and long-term function.
Complementary Therapies & PEMF
PEMF therapy (Pulsed Electromagnetic Field) is a game-changer:
- Reduces inflammation and pain
- Supports tissue, bone, and joint repair
- Boosts cellular energy and speeds healing
- Provides reassurance and control during recovery
Other complementary options:
- Acupuncture
- Massage therapy
- Guided stretching and yoga
- Nutrition and supplements
Tip: Combine complementary therapies with physical therapy and community support for holistic healing.
Quick Supporter Checklist
Before Surgery:
- Prep home for accessibility
- Pack essentials and comfort items
- Attend pre-op appointments
During Recovery:
- Help with mobility and daily tasks
- Encourage therapy participation
- Celebrate milestones
- Offer emotional support
Long-Term:
- Promote ongoing safe activity
- Maintain community connections
- Celebrate achievements
Recovery is a journey, but you don’t have to walk it alone. With preparation, support, and the right tools, you can reclaim mobility, confidence, and your life.
Call to Action:
- Join Hipster Club to connect with experienced patients
- Consider PEMF therapy as part of your recovery toolkit
- Prepare, support, and empower yourself—your healing journey is in your hands

You must be logged in to post a comment.