The Ultimate Guide to Hip Recovery: Preparing, Healing, and Thriving
This guide is your roadmap for navigating hip pain, preparing for surgery, recovering, and thriving afterward. It’s designed for anyone experiencing hip issues—whether it’s early-stage discomfort, post-surgery recovery, or long-term joint management.
Understanding Hip Pain and Joint Degeneration
Hip pain doesn’t always start suddenly. For many, it’s a slow progression…
- Early signs: Stiffness, mild pain, clicking or popping sounds
- Advanced signs: Bone-on-bone pain, loss of mobility, difficulty sleeping
- Common causes: Osteoarthritis, dysplasia, past injuries, autoimmune conditions
Why understanding your pain matters:
Many people try to push through discomfort, thinking it’s “normal aging.” But early recognition allows for interventions that can slow progression and improve quality of life.
Tip: Keep a pain and mobility journal. Track your daily activity, pain levels, and triggers. This record will help your doctor and physical therapist create a personalized plan.
Emotional and Mental Health in the Hip Journey
Hip pain is not just physical—it’s emotional. Many patients experience:
- Anxiety about mobility and independence
- Frustration with limitations in daily life
- Isolation from friends and activities they once enjoyed
Strategies to support emotional health:
- Mindfulness practices: Meditation, journaling, or guided imagery
- Community support: Hipster Club, support groups, and online forums
- Professional guidance: Physical therapists, counselors, or health coaches
- Set realistic goals: Celebrate small wins like walking further or sleeping through the night
Tip: Your mental health is directly linked to physical recovery. Don’t skip this part of your healing process.
Preparing for Hip Replacement Surgery
Preparation is key for a smooth recovery. Here’s a comprehensive checklist:
Physical Preparation
- Pre-op exercises to strengthen your core, glutes, and hip muscles
- Cardiovascular activity like swimming or cycling to improve endurance
- Stretching to maintain flexibility
Home Preparation
- Clear pathways, remove trip hazards, and place essentials within reach
- Set up a recovery station with pillows, water, and snacks
- Consider raised toilet seats, walkers, or supportive chairs
Medical Preparation
- Compile your medical history, medications, and supplements
- Ask your surgeon about blood work, imaging, and pre-op instructions
- Prepare questions about anesthesia, recovery timeline, and post-op therapy
Nutrition & Lifestyle
- Anti-inflammatory diet rich in protein, vegetables, and healthy fats
- Avoid alcohol and smoking to promote healing
- Hydrate well pre- and post-surgery
Tip: Think of this phase as building a foundation. The better you prepare, the smoother your recovery.
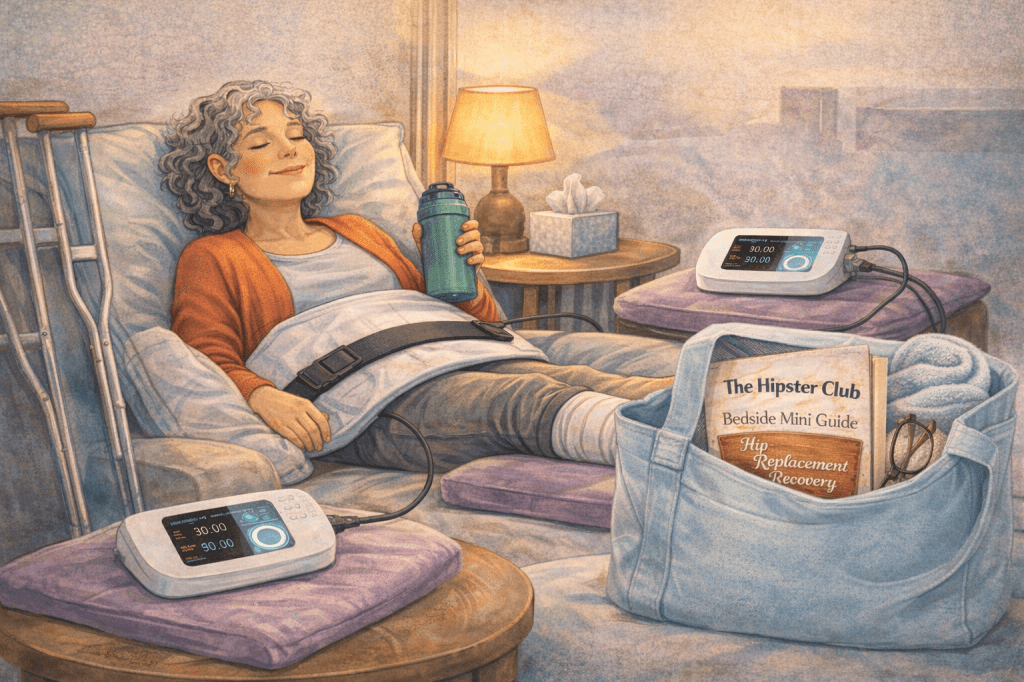
Post-Surgery Recovery Roadmap
Recovery is not one-size-fits-all, but there are key stages and strategies:
Immediate Post-Op (0–2 Weeks)
- Pain management: Ice, elevation, and medications as prescribed
- Movement: Gentle walking, short standing sessions
- Monitor for complications: Swelling, redness, fever, or unusual pain
Early Recovery (2–6 Weeks)
- Physical therapy begins: Strength and mobility exercises
- Gradual increase in activity: Walking, light chores, and gentle stretching
- Maintain mental health: Journaling and mindfulness to track progress
Mid-Recovery (6–12 Weeks)
- More active therapy: Swimming, cycling, and low-impact exercises
- Balance and stability: Core and leg strengthening
- Community engagement: Sharing progress, asking questions, learning from others
Long-Term Recovery (3–12 Months)
- Return to hobbies: Golf, walking, swimming, or light jogging
- Monitor hip health: Regular check-ins with your orthopedic surgeon
- Lifestyle adjustments: Weight management, posture awareness, and supportive footwear
Tip: Track your milestones and celebrate each stage. Recovery is a journey, not a race.
Nutrition & Supplements for Joint Health
What you eat directly affects your joints, inflammation levels, and recovery speed. Key considerations:
- Protein: Builds muscle to support hip stability
- Anti-inflammatory foods: Leafy greens, berries, turmeric, fatty fish
- Calcium & Vitamin D: Support bone density
- Magnesium & Omega-3s: Reduce inflammation and improve circulation
Supplement Tips:
- Talk to your doctor before starting new supplements
- Keep a food and symptom journal to track what works best
- Avoid excess sugar and processed foods that promote inflammation
Exercise & Movement Strategies
Movement is medicine—but it must be safe and tailored.
Low-Impact Options:
- Swimming and water aerobics
- Cycling on a stationary bike
- Walking on flat surfaces
- Yoga or Pilates (hip-friendly modifications)
Strengthening & Stability:
- Core exercises to protect the lower back and hips
- Glute activation to support hip stability
- Gentle resistance training with bands or light weights
Tip: Always listen to your body. Some days will feel better than others—progress gradually.
Community & Emotional Support
Recovery is easier with others who understand your journey. Hipster Club was built for this reason:
- Connect with people who’ve walked your path
- Share tips on surgery, recovery, and lifestyle adjustments
- Ask questions, celebrate wins, and get encouragement
Tip: Isolation slows healing. Even short check-ins or online discussions can make a huge difference.
PEMF Therapy: Boosting Recovery at the Cellular Level
Once your foundation—preparation, exercise, nutrition, and support—is in place, PEMF (Pulsed Electromagnetic Field) therapy can accelerate healing:
- Reduces inflammation – Eases pain and swelling in joints
- Supports cellular repair – Recharges ATP for energy and regeneration
- Enhances recovery – Promotes mobility and overall function
Types of Devices:
- Full-body mats: Energize all your cells
- Targeted paddles: Focus on hips, knees, or sore areas
- Brain-focused PEMF: Supports cognitive and neurological function
Tip: Think of PEMF as the “turbo boost” for your body—it complements therapy, movement, and lifestyle strategies.
Your Hip Recovery Checklist
- Educate yourself: Knowledge is power
- Track your progress: Pain, mobility, and emotional milestones
- Move with purpose: Consistency matters more than intensity
- Build your support network: Friends, family, or Hipster Club
- Advocate for yourself: Ask questions and explore holistic options
- Celebrate every win: Small improvements are still progress
- Explore PEMF therapy: Cellular support enhances all other recovery steps
Your Next Steps
- Join Hipster Club – Connect with others who understand your journey [Insert link]
- Schedule a consultation – Work with your healthcare provider on a personalized plan
- Try gentle exercises – Start walking, stretching, or swimming
- Learn about PEMF – Discover how targeted cellular energy can support your healing [Insert link]
Remember: Recovery is a journey, not a race. With preparation, support, and the right tools, you can reclaim your mobility, confidence, and life—one step at a time.
Download our Hipster Club Healing Workbook….below!





 Never ever in my wildest dreams would I have thought I would have needed a hip replacement. It started out as a
Never ever in my wildest dreams would I have thought I would have needed a hip replacement. It started out as a