Facing a hip or joint replacement can be an emotional rollercoaster. The physical pain is one thing—but the mental and emotional side can hit just as hard. You may find yourself spiraling into “what ifs,” fear, and even sadness about what’s to come. That’s completely normal—and it doesn’t mean you’re weak.
Acknowledge Your Feelings
The first step is simple but powerful: allow yourself to feel. Anxiety, sadness, fear, and even anger are natural reactions to the uncertainty of surgery. Suppressing them often makes them louder.
Try journaling:
- Write down your fears: “What if the pain doesn’t go away?”
- Write down your hopes: “I want to walk my dog pain-free again.”
- Write down what you can control: prepping your home, learning exercises, planning your recovery support.
“Naming your emotions gives them less power and helps you take the next step forward.”
Focus on Small Wins
Instead of letting your mind spiral to the endgame—surgery and recovery—focus on what you can do today:
- Take a short walk or stretch in a way that feels safe
- Prep your home for recovery (grab bars, pillows, a reachable water bottle)
- Connect with a friend or peer who has been through this
Even tiny actions remind your brain that you’re taking control, not just being swept along by fear.
Build a Pre-Surgery Support Team
You don’t have to carry this alone. Lean on your community:
- Friends & Family: Let them know exactly how they can help—rides, meals, check-ins.
- Hipster Club Members: Connect with someone who’s been through surgery and can share what to expect.
- Sponsor/Mentor: Ask questions about what the first week was like, and let them reassure you.
“Support isn’t a luxury—it’s a lifeline for your mental and emotional well-being.”
Practice Mindfulness & Stress Relief
Before surgery, stress reduction isn’t optional—it’s essential. Consider:
- Breathing exercises: 5–10 minutes of slow, deep breathing to calm the nervous system
- Meditation or visualization: Imagine yourself walking pain-free, or visualize your recovery process step by step
- Gentle movement: Safe stretching, swimming, or yoga (approved by your doctor) to release tension
- Journaling: Write letters to yourself about your fears and hopes
“Mind and body are connected. When one is calm, the other heals faster.”
Reframe the “What Ifs”
Your brain loves to play out worst-case scenarios—but you can challenge it:
- “What if it hurts?” → “Pain is temporary; I have a plan to manage it.”
- “What if recovery is slow?” → “Every step counts. I will ask for help and celebrate small victories.”
- “What if I lose independence?” → “I’m preparing, and I will regain my mobility and strength.”
This isn’t about ignoring fear—it’s about giving it structure and a path forward.
Connect to Purpose
Sometimes the darkest thoughts before surgery hide a bigger truth: you want your life back. Whether it’s walking the dog, dancing, swimming, or playing with grandchildren, anchor yourself in that “why.”
“Your goal isn’t just surgery—it’s reclaiming your life, one step at a time.”
Action Steps Before Surgery
- Write down your fears and hopes.
- Identify 3 people to lean on—friends, family, or a mentor.
- Prep your environment—make your home recovery-friendly.
- Schedule calming practices daily—breathing, meditation, gentle movement.
- Join a support community—ask questions, share concerns, and learn from others’ experiences.
Pre-Surgery Emotional Recovery Guide: Navigating the Days Before Your Joint Replacement
Facing a hip or joint replacement is a major life event. Beyond the physical preparations, your mind and emotions are going through a whirlwind: fear, doubt, anxiety, and sometimes even sadness. This guide is designed to help you navigate the emotional side of surgery, build confidence, and create a support system to carry you through recovery.
Step 1: Name Your Emotions
Before you can manage your feelings, you need to acknowledge them.
Exercise: Daily journaling prompt
- Write down everything you’re feeling—fear, sadness, anger, confusion, even guilt or frustration.
- Don’t censor yourself. No judgment. This is your space.
- Next to each feeling, write one small action you can take to respond:
Example:
- Fear: “I’m afraid of pain after surgery.” → Action: Research pain management strategies and talk to my PT.
- Anxiety: “I worry I won’t walk normally again.” → Action: Schedule pre-op exercises and read patient stories.
“Naming emotions gives you control over them instead of letting them control you.”
Step 2: Build Your Support Network
You don’t have to face surgery alone. Start connecting now.
Your Support Team:
- Sponsor / Mentor: Someone who has been through joint replacement. Ask for tips, reassurance, and real-world advice.
- Friends & Family: Identify 2–3 people who can help with meals, errands, or companionship during recovery.
- Healthcare Team: Surgeon, physical therapist, health coach—treat them as partners in your recovery.
Tip: Schedule a quick check-in with each person this week. Share what you need, and ask for guidance or support.
Step 3: Daily Mindfulness & Stress Relief
Stress before surgery is normal—but managing it helps both your mind and body.
Daily Practices:
- 5–10 minutes deep breathing: Inhale for 4, hold 2, exhale for 6. Repeat.
- Visualization: Picture your recovery—walking confidently, climbing stairs, returning to favorite activities.
- Gentle movement: Walking, stretching, or swimming (approved by your doctor).
- Journaling: Write about fears, hopes, and small victories.
“Mind and body are connected. When one is calm, the other heals faster.”
Step 4: Reframe Your ‘What Ifs’
Your brain loves worst-case scenarios. Challenge them with “what is” instead of “what if.”
Examples:
- “What if recovery is slow?” → “Recovery takes time. I will take it step by step.”
- “What if I lose independence?” → “I am preparing now and will regain my strength and mobility.”
- “What if pain is unbearable?” → “I have a plan and support for managing pain safely.”
Exercise: List your top 5 fears, and write one positive, actionable counter-thought next to each.
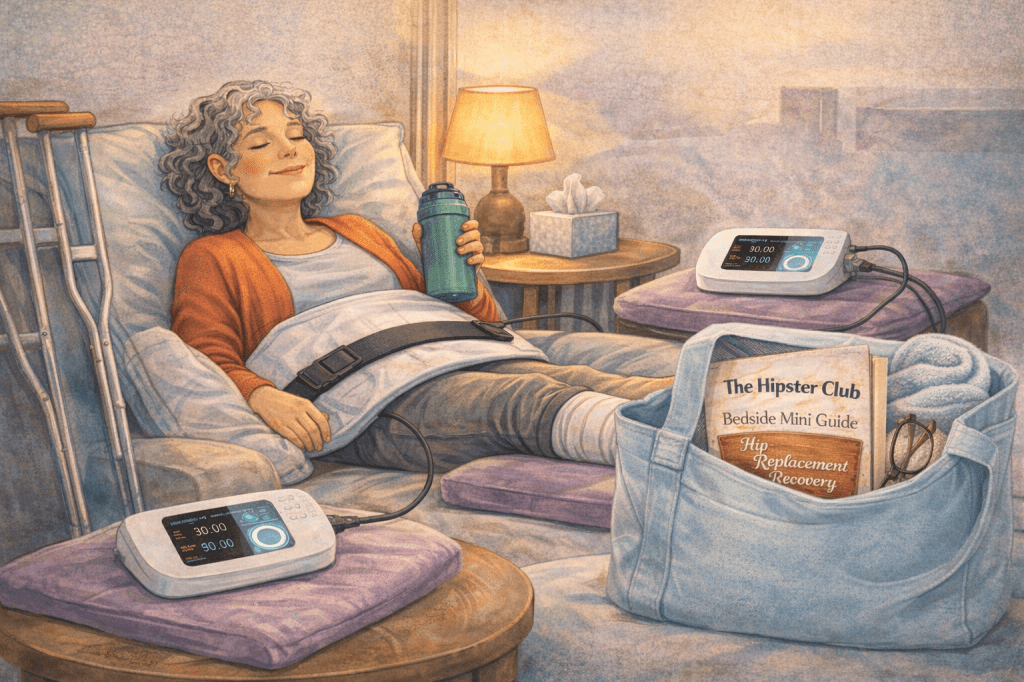
Step 5: Prepare Your Home & Recovery Space
Practical preparation reduces anxiety:
- Clear walkways and remove trip hazards
- Place essentials (water, snacks, medications) within reach
- Set up recovery station: comfortable chair, blankets, phone charger, reading materials
- Consider mobility aids: walker, cane, raised toilet seat
“The more ready your environment, the calmer your mind can be.”
Step 6: Connect with a Community
Supportive peers can provide reassurance, tips, and encouragement:
- Hipster Club or online forums: Ask questions, read recovery stories, and share your feelings.
- Local support groups: Some hospitals host pre-op or chronic pain sessions.
- Social media: Join small, private groups with like-minded people.
Tip: Don’t be afraid to ask the “small” or “silly” questions—chances are, someone else has wondered the same thing.
Step 7: Daily Reflection & Small Wins
Tracking progress and reflecting on small accomplishments builds confidence:
Example Tracker:
| Date | Emotion / Concern | Action Taken | Small Win / Positive Note |
|---|---|---|---|
| 11/30 | Anxiety | Breathing exercises | Felt calmer after 10 mins |
| 12/1 | Fear | Talked with mentor | Learned tips to prep for hospital |
| 12/2 | Overwhelm | Cleared recovery area | Felt more in control |
Tip: Celebrate any forward movement, no matter how small.
Step 8: Lean on Humor & Perspective
Surgery prep can feel heavy. A little humor goes a long way:
- Laugh at your “bionic body” fantasies
- Share funny stories about pre-surgery anxieties with friends
- Watch a lighthearted show or movie to distract your mind
“Healing starts in the mind. Humor is medicine for the soul.”
Step 9: Plan Your Post-Surgery Support
Knowing what to expect after surgery reduces pre-op anxiety:
- Daily routine: Meals, exercises, rest periods, medication schedule
- Check-ins: Plan calls with sponsor, friends, or family
- Milestones: Walking without pain, climbing stairs, resuming hobbies
Tip: Make a simple “recovery calendar” and include who will help and when.
Step 10: PEMF Therapy for Pre- & Post-Op Support
Many Hipster Club members find PEMF (Pulsed Electromagnetic Field) therapy useful both before and after surgery:
- Supports cellular healing
- Reduces inflammation and pain
- Enhances energy and recovery
- Complements physical therapy and lifestyle strategies
Tip: Discuss PEMF with your healthcare provider and consider incorporating it into your pre- and post-surgery plan for a holistic approach.
Your Pre-Surgery Checklist
✅ Name your emotions and journal daily
✅ Build a support network (sponsor, friends, family, healthcare team)
✅ Schedule mindfulness and stress relief practices
✅ Reframe “what if” thoughts
✅ Prep your home and recovery space
✅ Join a supportive community
✅ Track daily wins and milestones
✅ Use humor and perspective to lighten heavy moments
✅ Plan post-surgery support and routines
✅ Explore PEMF therapy as part of holistic recovery
Final Words
The days leading up to surgery can feel heavy—but they are also a chance to prepare mentally, emotionally, and physically. Building your community, leaning on your support system, and creating practical routines will give you confidence and calm as you take this important step toward reclaiming your life.
“You are not alone, you are not helpless, and you are stronger than you know. With the right support, preparation, and mindset, you can face surgery—and recovery—with courage and hope.”
Feeling anxious or sad before surgery is not a weakness—it’s a natural response to a major life event. By acknowledging your emotions, leaning on your community, and practicing small daily steps to manage stress, you can face surgery with more confidence, clarity, and courage.
“You’re stronger than you think, and you don’t have to walk this path alone. Reach out, prepare, breathe—and remember, your future self will thank you.”